Full HTML
Prevalence of tuberculosis in Shabwah Governorate, Yemen: A cross-sectional study
Hesham Saeed Hezam, Saleh Hussein Humaidah
Author Affiliation
1Consultant and Head, Department of Medicine, Ataq General Hospital, Shabwah Governorate, Yemen,
2Radiology Technician, Coordinator of the National Tuberculosis Program, Shabwah Governorate, Yemen
Abstract
Background: There is a lack of data on current tuberculosis (TB) burden in Shabwah Governorates in Yemen. This study aimed to investigate the prevalence, epidemiology, and outcomes of TB disease in Shabwah Governorate, Yemen. Materials and Methods: This cross-sectional study was conducted at the National TB Program (NTP) Center in Ataq City, Shabwah Governorate, Yemen. The study involved TB patients of different ages who were notified at the center between January 1, 2021, and December 31, 2021. Results: We involved a total of 123 new active TB cases, including 86 (69.9%) with pulmonary TB (PTB) and 37 (30.1%) with extrapulmonary TB (EPTB). The total prevalence of TB disease during the year 2021 was 14.5 new TB cases per 100,000 population, while the median age of the study population was 34 years. The majority of the cases (23.6%) belonged to age group 15–24 years. There was a slightly higher preponderance of males 54.5% (n=67). EPTB was detected in 37 (30.1%) patients with lymph nodeTB being the most common manifestation [17 (46.0%)]. All patients received four-drug anti-TB therapies for 6–12 months. Most patients 111 (90.3%) were cured, and 2 (1.6%) patients died during the course of the disease, while 10 (8.1%) patients were lost during follow-up. Conclusion: The prevalence of TB in Shabwah Governorate was 14.5/100,000 population. Male patients and younger age groups were more affected, while the lymph nodes were the main extrapulmonary sites involved and the cure rate was 90.2%. The results of the study indicate the need to revise the notification form for active TB cases and to expand NTP activities to focus on targeted screening for active TB cases in high-risk groups to close the gap in unidentified TB cases.
DOI: 10.32677/yjm.v1i1.3447
Keywords: Acid-fast bacilli, Extrapulmonary tuberculosis, Prevalence, Pulmonary tuberculosis
Pages: 36-37
View: 18
Download: 40
DOI URL: https://doi.org/10.32677/yjm.v1i1.3447
Publish Date: 27-03-2025
Full Text
Tuberculosis (TB) remains a major health problem in lowincome countries, and one of the leading causes of death worldwide. According to the World Health Organization (WHO), 10 million people contracted TB in 2020, with 1.5 million deaths worldwide [1]. More than a third of estimated TB cases are expected to be missed by notification, contributing significantly to TB transmission in communities and driving the global TB epidemic. The WHO estimate of the TB incidence rate is based on case notification and expert judgment [2].
Yemen has a moderate TB burden. According to the WHO estimates, 14,700 TB patients were reported in Yemen in 2020, with an incidence rate of 49/100,000 people and a mortality rate of 7.3.100,000 people [3]. It should be noted that the only source of data on the number of TB cases in the country is the National TB Program (NTP), which was established in 1970 [4]. Due to the civil war, Yemen currently suffers from poverty and social unrest, which are factors that seriously affect TB infection rates. Considering that, most NTP centers do not conduct national TB prevalence surveys to estimate new TB cases due to fund constraints [4], the number of TB cases announced by the WHO in Yemen, especially after the outbreak of the civil war, is controversial. In addition, many people in remote areas of the country have not been able to access the NTP facilities due to logistical or financial barriers, while some patients, particularly in the north of the country, have been able to obtain diagnostic and treatment services from the private sector and thus both missed from notification. Therefore, we believe that the actual cases of active TB in the country have been underreported.
Although NTP has several offices in every governorate across the country, there is a lack of publications on the current active TB burden in each governorate, especially after the outbreak of the civil war. This study aimed to highlight the prevalence, epidemiology, and outcomes of TB disease in Shabwah Governorate, Yemen.
MATERIALS AND METHODS
Design, Population, and Setting
This descriptive cross-sectional study was conducted at the NTP Center in Ataq City, Shabwah Governorate, Yemen. This center notifies TB cases from different districts of Shabwah Governorate and offers acid-fast bacilli (AFB) smear testing, chest X-ray, and anti-TB drugs free of charge. The NTP adopted the WHO Stop TB Strategy, which focused on the extension of basic Directly Observed Therapy Short-course services. The study involved TB patients of different ages who were notified in the center between January 1, 2021, and December 31, 2021.
Definitions and Inclusion Criteria
The study involved patients of different ages, who were diagnosed with active TB disease by their treating physicians. Two forms of active TB were recognized, pulmonary TB (PTB) and extrapulmonary TB (EPTB). Based on the identification of AFB on microscopic examination of unconcentrated sputum, PTB patients were divided into smear-positive PTB and smearnegative PTB. Patients with at least two sputum smear-positive for AFB by direct smear microscopy were diagnosed with smearpositive active PTB, while subjects who were smear-negative but had clinical and/or radiological findings suggestive of PTB and responded adequately to anti-TB treatment were considered to have clinically diagnosed active PTB.
EPTB involved TB disease of any organ other than the lung parenchyma. EPTB was diagnosed by bacteriology/histology of aspirated/biopsied specimen. Bacteriology of aspirated/biopsied specimen included smear for AFB only as polymerase chain reaction (PCR) test to DNA of Mycobacterium TB (MTB), and TB culture facilities were not available in the governorate. Cases of EPTB that had not been confirmed by bacteriology/histology of an aspirated/biopsied specimen, but had clinical, radiological findings, and/or fluid analysis suggestive of EPTB and adequately responded to anti-TB treatment were considered to have clinically diagnosed EPTB.
TB treatment was defined as the use of four anti-TB medications for not <6 months divided into intensive and continuation phases. Lost to follow-up is defined as a case whose treatment was interrupted for 2 consecutive months or more after the last medicine intake. Cure is defined as a TB patient who has completed the duration of treatment and has at least one sputum smear-negative or clinical improvement at the end of treatment. Death is defined as a patient who died from any cause while being treated for TB.
Data Analysis and Ethical Approval
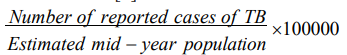
We used a simple descriptive statistic. Data were reported as median [Interquartile range (IQR)] for quantitative variables, whereas qualitative variables were described as numbers and percentages. The following formula was used for estimating the prevalence of TB [5]:
The permission to conduct this study was obtained from a local authority as there is no research entity in the governorate to obtain ethical approval.
RESULTS
During the period from January 1, 2021, to December 31, 2021, the information system of the NTP center in Shabwah Governorate reported a total of 123 new TB cases, including 86 (69.9%) with PTB and 37 (30.1%) with EPTB. The total prevalence of TB disease during the year 2021 was found to be 14.5 new TB cases per 100,000 population, while the median age of the study population was 34 years (IQR: 20–35 years). The majority of the cases (23.6%) belonged to the age group 15–24 years. There was a slightly higher preponderance of males 54.5% (n=67), and most of the patients 75 (61.0) were identified in Ataq district. Table 1 describes the demographic and clinical characteristics of the study population. In addition, the distribution of TB patients in the different districts of Shabwah Governorate is summarized in Table 2.
Of the 86 cases with PTB, AFB microscopy was positive in 24 (27.9%) cases, while 62 (70.1%) cases were diagnosed clinically. All EPTB cases were diagnosed outside the governorate and referred to our center for notification and management. EPTB was detected in 37 (30.1%) patients with lymph node TB being the most common manifestation [17 (46.0%)], followed by pleural TB 8 (21.6%) patients, spinal TB 5 (13.5%) patients, central nervous system TB 4 (10.8%) cases, abdominal TB 2 (5.4%), and nasopharyngeal TB 1 (2.7%) patient (Table 1). All patients received four-drug anti-TB therapies; 101 (82.1%) cases received anti-TB therapy for 6 months and 12 (9.8%) patients received anti-TB therapy for 9–12 months. The treatment was supervised directly by NTP staff from initiation until completion. Most patients 111 (90.3%) were cured after completion of treatment, and 2 (1.6%) patients died during the treatment, while 10 (8.1%) patients were lost during follow-up (Table 1).
DISCUSSION
TB remains a major public health problem in developing countries such as Yemen, where NTP is the main health entity that deals with active TB cases. Before the outbreak of the civil war, the NTP budget was provided by international donors to the ministry of public health and population to cover NTP activities across the country [4]. However, as of 2015, the International Organization for Migration (IOM) has become the intermediary between international donors and the NTP in Yemen.
Describing the epidemiology of TB in any country is crucial for policymakers to put the appropriate strategies to prevent the disease and decrease the global burden of TB. To the best of our knowledge, no previous study has documented the epidemiology of active TB disease in Shabwah Governorate. However, this study was conducted under difficult circumstances in the country, where the civil war and resulting humanitarian crises have led Yemen’s health authorities to focus on victims of the war at the expense of other health issues such as improving health facilities and programs. In Shabwah Governorate, although the local authority has supported the NTP by holding workshops and symposiums to improve and expand staff skills and knowledge about TB, there is still a shortage of diagnostic facilities such as PCR tests for MTB DNA and TB culture. TB infection in humans is mainly caused by MTB complex. The data on the causative pathogens for TB were however not available to this study, because PCR test to DNA of MTB, and TB culture facilities were not available in the governorate. However, we believe that our findings are novel and of interest.


The information system of the NTP center in Shabwah Governorate reported a total of 123 new TB cases with a prevalence of 14.5 new cases per 100,000 population in 2021, which is low compared to some studies from developing countries. In Kashmir Valley [5], the prevalence of TB in 2020 was 37.31/100,000 population, almost double the figure in our study. For unknown reasons, the present study showed a male predilection, which is in line with many studies worldwide [2,6-9], but in contrast to a few studies from Pakistan [10,11]. Similar to studies from Kashmir [5], and Rawalpindi [12], the most TB cases in this study were reported in the 15–24 age group, suggesting that TB disease in Shabwah is driven by increased exposure as well as the progression of untreated latent TB. Significantly, there is a variation in the frequency of EPTB in different studies. The estimated proportion of EPTB in our study was 30.1%, which is similar to that from Spain (32.6%) [8], China (33.4%) [9], and Pakistan (29.2%) [10], but, higher than other studies from Sudan (21.0%) [13], Brazil (13.0%) [14]. The proportion of EPTB in the present study is lower than in other developing countries such as Algeria (43.8%) [15] and India (41.7%) [16]. One of the reasons for the variation in estimates of EPTB epidemiology is a difference in terminology. Some authors regard pleural TB as a form of EPTB, while others consider the lung and their covering pleura as PTB, and use the term extrathoracic TB or extrarespiratory TB instead of EPTB to describe TB of all organs except the thorax [17]. A review of the literature revealed that there is variation in the sites of EPTB among various studies. We found that the most frequent site of EPTB was the lymph node, which is consistent with findings from Sudan [13], Nepal [18], Algeria [15], Spain [8], and Turkey [19]. In Pakistan, India, and Madagascar [10,16,20], the pleura was the most common site of extrapulmonary involvement; however, disseminated TB was shown to be the common form of EPTB in Ghana [21]. In the USA and China [9,22], bones and/or joints were the most common EPTB sites involved. The reasons for these discrepancies were unknown. Interestingly, we observed that all notified EPTB cases at our center were diagnosed outside the governorate, suggesting a lack of diagnostic facilities in the governorate, which prompted people to seek additional resources in major cities, where the private sector provides the necessary facilities. Regarding the treatment outcomes, the cure in our study was 90.3%, which is high compared with that of many studies in developing countries such as Ethiopia [2], India [5], and Pakistan [11], reflecting the efficacy of the NTP in our governorate, which demonstrated organized TB control activities. As noted, our current activities within the NTP have focused on the diagnosis, notification, and treatment of active TB cases that were referred from other health-care facilities in the governorate. This situation calls for expansion of our activities to include new scientific approaches focused on targeted screening for active TB disease among the high-risk groups in the governorate through regular surveillance activities. The use of X-pert MTB/RIF ultra assay should also be considered for TB disease diagnosis at the NTP center to enable an early diagnosis to cut the ongoing transmission and to allow timely and appropriate disease management. A failure to address these issues will have serious implications in terms of the further spread of TB disease in the governorate. Our study had several limitations. First, the study is retrospective, and it was confined to one governorate of the country. Second, there was a lack of data on clinical presentation and risk factors such as smoking, alcohol use, and diabetes mellitus. Because the notification form provided by the main office of NTP in Aden city does not include these variables. Third, the data on the causative pathogens for TB were not available to this study, because PCR test to DNA of MTB, and TB culture facilities were not available. Finally, the present study did not investigate the HIV serology due to lack of diagnostic kits. HIV serology is quite important to be performed since HIV is common among TB patients. Despite these limitations, our study is the first to describe the epidemiology of TB in Shabwah governorate and, thus, provides baseline data for assessing the impact of disease control and for future assessments of epidemiological trends in the governorate.
CONCLUSION
This study showed that the prevalence of TB in Shabwah governorate was 14.5/100,000 population. Male patients and younger age groups were more affected, with the lymph nodes being the main extrapulmonary site involved, and 90.3% of cases were cured. The results of the study demonstrate the need to revise the active TB case notification form to include more important variables. Closing the gap in unidentified TB cases requires an expansion of NTP activities to focus on targeted screening for active TB cases among high-risk groups in the governorate through regular surveillance activities. Despite the strong support that the NTP in Shabwah Governorate has received from the local authority and external donors, we believe that continued government support for TB control activities, both technically and financially, is needed to achieve TB elimination goals in Yemen. In addition, further studies in other governorates across the country are needed to identify the areas with the highest TB burden at the regional levels to aid TB program supporters to reallocate the limited resources accordingly.
AUTHORS’ CONTRIBUTION
Hezam HS analyzed the data, reviewed the literature, and wrote the final manuscript. Humaidah SH aided in the data collection, literature review, data entry, and revision of the final manuscript. All authors read the manuscript and agree to its publication.
References
1. Global Tuberculosis Report 2021: Available from: https://www.who.int/ publications/i/item/9789240037021 [Last accessed on 2022 Apr 01].
2. Deribew A, Deribe K, Dejene T, et al. Tuberculosis burden in Ethiopia from 1990 to 2016: Evidence from the global burden of diseases 2016 Study. Ethiop J Health Sci 2018;28:519-28.
3. The World Bank. Available from: https://www.data.worldbank.org/indicator/ SH.TBS.INCD?locations=YE [Last accessed on 2022 Apr 01].
4. Al Kalali FS, Mahyoub E, Al-Hammadi A, et al. Evaluation of the national tuberculosis surveillance system in sana’a, Yemen, 2018: Observational study. JMIR Public Health Surveill 2021;7:27626.
5. Puttoo AN, Shah NN, Tripathi S, et al. Prevalence of tuberculosis in the North Indian subcontinent Kashmir valley: A cross-sectional hospital-based study. J Clin Diagn Res 2022;16:10-4.
6. Abdallah TM, Ali AA. Epidemiology of tuberculosis in Eastern Sudan. Asian Pac J Trop Biomed 2012;2:999-1001.
7. Elsafi SS, Nour BM, Abakar AD, et al. Pulmonary tuberculosis among Sudanese individuals of White Nile state: Prevalence and role of the sociodemographic features and laboratory findings in the assessment of infection. J Microbiol Exp 2020;8:52-63.
8. García-Rodríguez JF, Álvarez-Díaz H, Lorenzo-García MV, et al. Extrapulmonary tuberculosis: Epidemiology and risk factors. Enferm Infecc Microbiol Clin 2011;29:502-9.
9. Pang Y, An J, Shu W, et al. Epidemiology of extrapulmonary tuberculosis among inpatients, China, 2008-2017. Emerg Infect Dis. 2019;25:457-64.
10. Tahseen S, Khanzada FM, Baloch AQ, et al. Extrapulmonary tuberculosis in Pakistan-a nation-wide multicenter retrospective study. PLoS One 2020;15:0232134.
11. Jehangir F, Hashmi R, Lateef TK, et al. Prevalence and outcomes of tuberculosis treatment in a primary care center in Karachi, Pakistan. Arch Med 2020;12:1-6.
12. Fatima R, Ejaz Q, Enarson DA, et al. Comprehensiveness of primary services in the care of infectious tuberculosis patients in Rawalpindi, Pakistan. Public Health Action 2011;1:13-5.
13. Abdallah TM, Toum FE, Bashir OH, et al. Epidemiology of extra pulmonary tuberculosis in Eastern Sudan. Asian Pac J Trop Biomed 2015;5:505-8.
14. Gomes T, Reis-Santos B, Bertolde A, et al. Epidemiology of extrapulmonary tuberculosis in Brazil: A hierarchical model. BMC Infect Dis 2014;14:9.
15. Selmane S, L’Hadj M. Epidemiology and clinical characteristics of tuberculosis in leon bernard tuberculosis unit in Algeria. Int J Mycobacteriol 2020;9:254-60.
16. Prakasha SR, Suresh G, D’sa IP, et al. Mapping the pattern and trends of extrapulmonary tuberculosis. J Glob Infect Dis 2013;5:54-9.
17. Kulchavenya E. Extrapulmonary tuberculosis: Are statistical reports accurate? Ther Adv Infect Dis 2014;2:61-70.
18. Sreeramareddy CT, Panduru KV, Verma SC, et al. Comparison of pulmonary and extrapulmonary tuberculosis in Nepal-a hospital-based retrospective study. BMC Infect Dis 2008;8:8.
19. Musellim B, Erturan S, Duman ES, et al. Comparison of extra-pulmonary and pulmonary tuberculosis cases: Factors influencing the site of reactivation. Int J Tuberc Lung Dis 2005;9:1220-3.
20. Razanamparany VR, Ménard D, Aurégan G, et al. Extrapulmonary and pulmonary tuberculosis in antananarivo (Madagascar): High clustering rate in female patients. J Clin Microbiol 2002;40:3964-9.
21. Ohene SA, Bakker MI, Ojo J, et al. Extra-pulmonary tuberculosis: A retrospective study of patients in Accra, Ghana. PLoS One 2019;14:0209650.
22. Yang Z, Kong Y, Wilson F, et al. Identification of risk factors for extra pulmonary tuberculosis. Clin Infect Dis 2004;38:199-205.
