Full HTML
Impact of COVID-19 pandemic on stroke rate, risk factors, clinical presentation, and outcome, in Hadramout, Republic of Yemen
Rasheed Mohammed Bamekhlah1, Samira Awad Banser2, Saeed Salim Binnoob3, Nasser Mansoor Habtor3, Saeed Abobaker Othman3, Fatima Jumaan Bin Neser3
Author Affiliation
1Professor of Internal Medicine, Senior Consultant, Department of Medicine, College of Medicine and Health Sciences (HUCOM), Hadramout University,
2Medical Specialist,
3Resident, Department of Medicine, Ibn-Seena Teaching Hospital, Mukalla, Hadramout, Yemen
Abstract
Background and Objective: The COVID-19 pandemic affected medical care systems including stroke care, globally. In this study, we investigated the impact of the COVID-19 outbreak on stroke care in Hadramout, in terms of rate of admission, access to care, risk factors, clinical presentation, and outcome. Methods: A hospital-based cross-sectional study comparing all stroke patients admitted to Ibn-seena University Hospital (ISTH), Mukalla, Hadramout, during two periods, May 1 to October 31, 2020, during the pandemic of COVID-19 (COVID-19 group), and from May 1 to October 31, 2019 (pre-COVID-19 group). Data collected from patients' medical record files into a master sheet, and were processed by the Statistical Package for Social Sciences (SPSS) software. Results: There were 117 stroke patients admitted in COVID-19 pandemic in 2020, and 213 patients admitted in the same period in 2019. Stroke admission declined by 45.1% (Odds Ratio(OR)=0.30, 95% confidence interval(95% CI): 0.22-0.42, P<0.0001). with no age and sex differences. Hypertension and diabetes mellitus were more frequent in COVID-19 group than the pre-COVID-19 group (OR=1.74, 95% CI: 1.08-2.80, P=0.02) and (OR=1.81, 95% CI: 1.14-2,88, P=0.01] respectively. No significant difference in other risk factors was found. Patients in COVID-19 group arrived the hospital more late than the patients in pre-COVID-19 group (OR=2.63, 95% CI: 1.64-4.21, P<0.0001). Dysphasia and altered consciousness including coma were more common in COVID-19 group compared with pre-COVID-19 group (OR=4.5, 95% CI: 2.18-9.08, P<0.0001) and (OR=3.2, 95% CI: 2.00-5.12, P<0.0001) respectively. Hospital stay was greatly reduced among COVID-19 group as compared with pre-COVID-19 group (02.9±0.31 days vs. 8.6±0.92 days, P<0.0001) Mortality rate was higher among COVID-19 group than the pre-COVID-19 group (41.9% vs. 27.2%, P=007). Conclusion: The number of stroke patients admitted during the COVID-19 pandemic decreased, they arrived late and spent shorter hospital stays while having higher rates of hypertension, diabetes, and impaired consciousness with a high mortality rate.
DOI: 10.32677/yjm.v2i1.3839
Keywords: Cerebrovascular accident, COVID-19, Hadramout, Stroke, Yemen
Pages: 25-29
View: 4
Download: 7
DOI URL: https://doi.org/10.32677/yjm.v2i1.3839
Publish Date: 10-05-2023
Full Text
INTRODUCTION
The COVID-19 pandemic severely impacted medical care systems, requiring a significant restructuring of services to ensure continuity of care for patients [1]. Recent studies have demonstrated certain negative impacts of the outbreak on acute stroke care, particularly during the first wave of the COVID-19 pandemic [2,3], which has resulted in a decrease in emergency department admissions for non-vascular disease, stroke, and cardiovascular disease recorded. There is no evidence that stroke patients are more (or less) vulnerable to COVID-19. However, patients with COVID-19 can develop a new stroke and the neurological symptoms of COVID-19 could potentially complicate stroke detection [4], also COVID-19 is associated with a hypercoagulable state that can lead to an increase in acute cerebrovascular events with an increase in ischemic strokes and strokes due to occlusion of large vessels [5-7].
Yemen has experienced three waves of the COVID-19 pandemic [8], the impact of which on the healthcare system has been studied [9]. However, the extent to which stroke care has been affected by this pandemic is unknown. This study was designed to assess the impact of the COVID-19 outbreak on stroke care in Hadramout Governorate in terms of admission rate, access to healthcare, risk factors, clinical presentation, and outcome.
Materials and methods
Study Design, setting, and population
We conducted a hospital-based retrospective analytic cross-sectional study involving all stroke patients admitted to Ibn-seena Teaching Hospital (ISTH), Mukalla, Hadramout, Republic of Yemen over two periods. The first period began on May 1. until October 31. 2020 during the COVID-19 pandemic (COVID-19 group), with the second period starting on May 1. to October 31. 2019 (pre-COVID-19 group) for comparison. The hospital is the largest tertiary referral center in Hadramout Governorate, where students from health and medical institutes get their training and provide healthcare for some 4,000,000 people in eastern Yemen.
Data source and data collection:
Data were collected by a trained group of medical graduates and students from patients' medical records into a master sheet based on the World Health Organization's (WHO) Stepwise Approach to Stroke Surveillance (STEPS-stroke) protocol and including age, gender, risk factors, clinical presentation, and outcome.
Statistical Analysis:
Data were processed using Statistical Package for Social Sciences (SPSS) software version 20.0 (IBM Corporation, Armonk, NY, USA). Categorical variables were described with their absolute frequencies and percentages. To compare the proportion of categorical data, we used the chi-square test and, where appropriate, Fisher's test. Student's t-test for independence was used to compare the numerical data. The confidence interval (CI) was set at 95% and the odds ratio (OR) was used when appropriate. The level of statistical significance was set at 5% and the difference was considered significant if p<0.05.
Ethical Consideration:
Permission to conduct this study was obtained from the hospital administration as there is no research committee in the governorate to obtain ethical approval.
Results
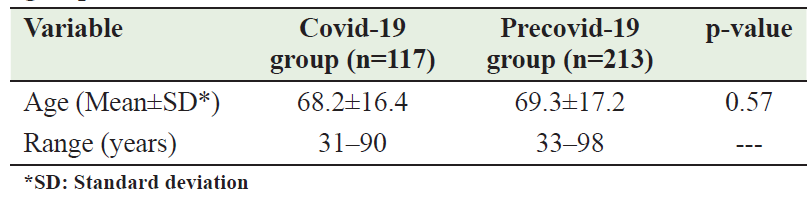
In 2020, 117 stroke patients were admitted during the COVID-19 pandemic (COVID-19 group) and 213 patients were admitted during the same period in 2019 (pre-COVID-19 group). Patients in the COVID-19 group accounted for 54.9% (117/213) of patients in the pre-COVID-19 group, resulting in a 45.1% reduction in stroke rate, which was statistically significant (OR=0.30, 95% CI: 0.22-0.42, P <0.0001). However, the difference in mean ages between the COVID-19 group (68.2±16.4) and the pre-COVID-19 group (69.3±17.2) was not statistically significant (p = 0.57). [Table 1].
Table 1: Age distribution of COVID‑19 and pre‑COVID‑19 period groups
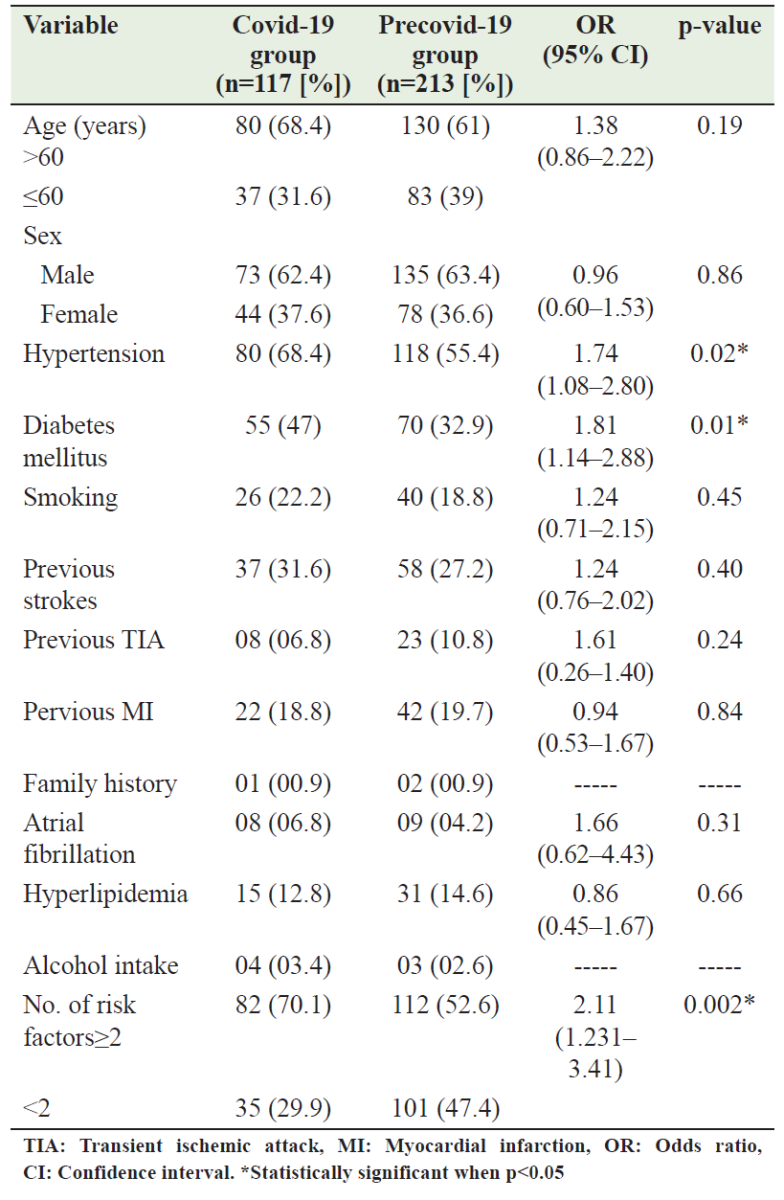
Patients older than 60 years were more in the COVID-19 group than in the pre-COVID-19 group (68.4% vs. 61%), but there was no statistically significant difference between the two groups (OR=1.38, 95% CI: 0.86-2.22, P=0.19); likewise, there was no statistically significant difference between the sexes in both groups (OR=0.96, 95% CI: 0.60-1.53, P=0.86). Hypertension (HTN) and diabetes mellitus (DM) were significantly more frequent in the COVID-19 group than in the pre-COVID-19 group (OR=1.74, 95% CI: 1.08-2.80; P=0.02) and (OR=1.81, 95% CI: 1.14-2,88; P=0.01] respectively. However, atrial fibrillation, smoking, alcohol use, history of seizures, history of transient ischemic attack (TIA), history of acute myocardial infarction, hyperlipidemia, and family history did not show significant differences between the two groups. Compared to the other group, patients in the COVID-19 group were more likely to have two or more risk factors (70.1 % vs. 52.6%) with statistically significant differences (OR=2.11, 95% CI: 1.231-3.41, P=0.002). [Table 2].
Table 2: Risk factors of stroke in the COVID‑19 period and pre‑COVID‑19 period groups
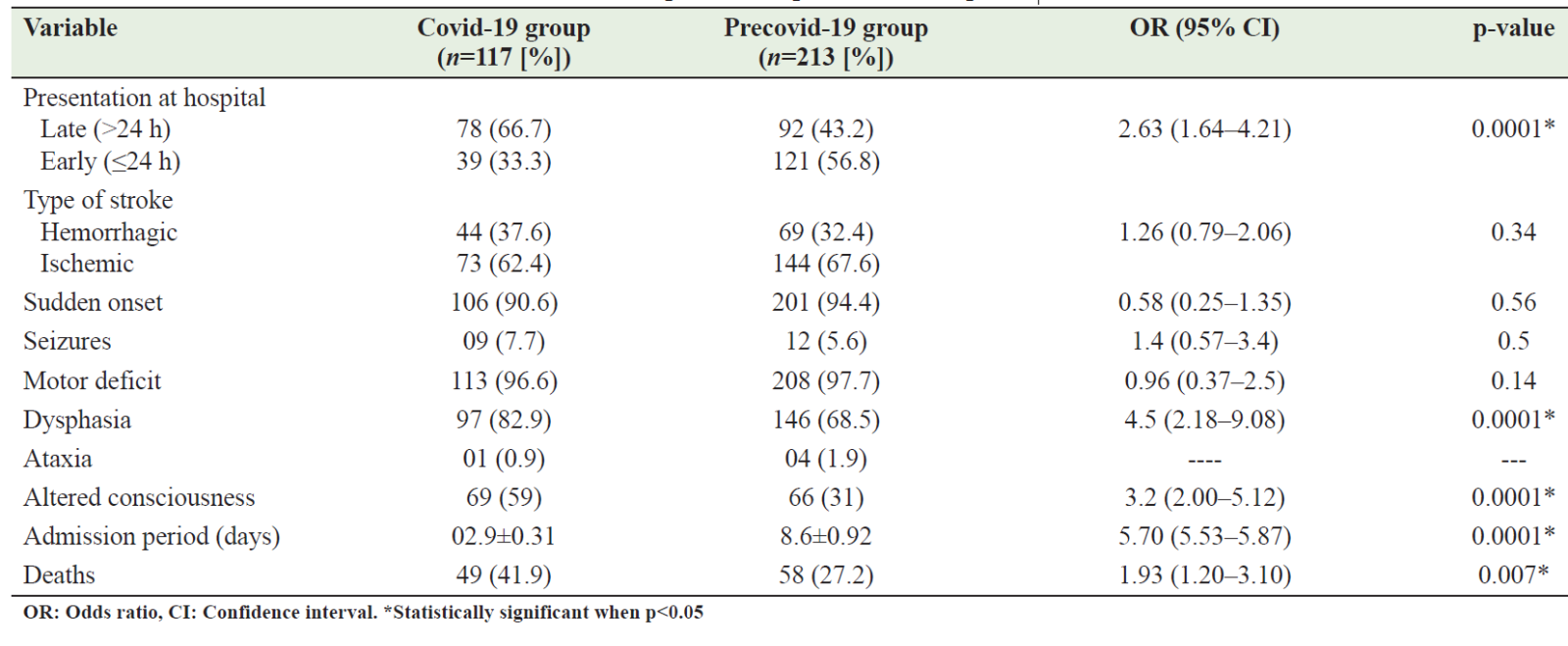
In the COVID-19 group, more patients arrived at the hospital >24 hours after the attack than in the other group (66.7% vs 43.2%), with statistically significant differences (OR =2.63, 95% CI: 1, 64 -4.21, P <0.0001). The types of stroke (ischemic vs. hemorrhagic) experienced by the two groups did not differ significantly from each other (OR=1.26, 95% CI: 0.79-2.06, P=0.34). likewise, there were no significant differences between both groups in terms of the onset of strokes, seizures, motor deficits, and ataxia. On the other hand, patients in the COVID-19 group were significantly more likely to experience dysphasia than those in the other group [(82.9% vs 58.5%), OR=4.5, 95% CI: 2.18-9.08, P <0.0001]. Moreover, altered consciousness, including coma, also was demonstrated more in the COVID-19 group than the other group with significant differences [(59 vs. 31%), OR=3.2, 95% CI: 2.00-5.12, P< 0.0001]. Hospitalization time was significantly shorter in the COVID-19 group compared to the pre-COVID-19 group [(02.9±0.31 vs 8.6±0.92 days), OR=5.70, 95% CI: 5.53-5.87, P< 0.0001]. There were significant differences between the TWO groups in terms of deaths, which were higher among patients in the COVID-19 group than the other group [(41.9% vs. 27.2%), OR=1.93, 95% CI: 1.20-3.10, P= 0.007]. [Table 3].
Table 3: Clinical data of stroke Patients in the COVID‑19 period and pre‑COVID‑19 period
DISCUSSION
The COVID-19 pandemic has had a major impact on healthcare systems worldwide. The outbreak led to an increase in the number of acute respiratory cases presenting to hospitals and eventually to intensive care units and also affected admissions and care for other illnesses. Most countries, including Yemen, implemented curfews or lockdowns as well as preventive measures to reduce the burden of the disease. Such measures had an impact on the level of care given to patients with other acute illnesses [10,11].
There was a noticed decline in stroke hospitalization rate during the COVID-19 pandemic. Our study revealed a significant reduction (45,1%), which was higher than several studies worldwide (26-40.4%) [12-21], other studies showed the same, but it was not significant (9-29%) [22-24]. Samkari et al., in Saudi Arabia, attributed this non-significance to the small number of patients involved [22], however, the West Midlands Ambulance Service University NHS Foundation Trust Ambulance Service, which covers the Royal Stoke University Hospital and the wider West Midlands region, reported no reduction in callouts for stroke [25]. On the other hand, John et al. showed a 41.9 percent increase in stroke patients during the COVID-19 pandemic, which was attributed to centers ceasing to treat these patients during the pandemic [26].
The COVID-19 pandemic caused a significant delay between stroke onset and patient arrival at the hospital [27-29]. Similarly, we reported that stroke patients who arrived at the hospital 24 hours after stroke onset during the COVID-19 period were more than those in the pre-COVID-19 period (66.7% vs. 43.2 %, p<0.0001). On the other hand, in Saudi Arabia, it was found that before the COVID-19 pandemic, the mean duration of symptoms before arrival at the hospital was 21.9 hours, while it had decreased to 8 hours during the pandemic (p=0.032). The authors suggested that this may be related to the increased use of the Red Crescent during the curfew time [22].
The age and gender distribution of the patients did not differ between the two periods, as our study and most relevant studies had shown [14,16,23,28-32]. However, Rameez et al., in the United States, when studied the impact of a stay-at-home order on stroke admission, found that stroke patients admitted during the COVID-19 period were younger than those during the pre-COVID-19 one [ 33], while Samkari et al. in Saudi Arabia reported a decrease in the number of female patients during the COVID-19 period [22].
In contrast to other studies [14,16,20,22,24,32,33], our study found that the number of patients with hypertension and diabetes mellitus was high during the COVID-19 pandemic compared to patients in the pre-COVID-19 era, consistent with Teo et al. Results [29]. In Yemen, war-related stress was exaggerated by the COVID-19 pandemic, which may explain in part our findings.
Due to the lockdown and fear of contracting COVID-19, people kept their stroke patients at home and tried to treat them traditionally until their condition worsened, causing patients to present with more severe symptoms when hospitalized. Dysphasia was documented more among stroke patients in the COVID-19 group compared with those in the pre-COVID-19 group (82.9 vs 68.5%, p< 0,0001), altered consciousness including coma also, is a serious presentation in stroke, we reported that it was higher among COVD 19 group patients than in the preCOVID-19 group (59% vs 31%, p<0.0001), which is in agreement with Wallace et al [32], however, Kwan et al. did not find any differences in the median of Glasgow coma scale between the two groups [34]
In our study, we found that the hospitalization period of stroke patients during the pandemic period was less than in the pre-pandemic one, (02.9±0.31 and 8.6±0.92 days respectively, p 0.007), which is consistent with many other studies [23,24,28]. In line with many other studies [23,24,28], we found that the hospitalization time for stroke patients during the pandemic period was shorter than in the pre-pandemic one (02.9±0.31 days vs 8.6±0.92 days, p=0.007). We also reported that in-hospital mortality increased among patients who presented with altered consciousness including coma, compared with patients who presented fully conscious; which coincides with many reports worldwide [35-37].
This study has some limitations. First, it is a retrospective study, which limited our access to some variables such as the reason for late arrival at the hospital, and stroke severity, due to incomplete medical records, moreover, patient follow-up was not feasible as we mainly depend on the patient’s medical records. Second, because this was a hospital-based study, the results could not be extrapolated to other settings. Despite these limitations, we believe that our data are the first to describe the impact of the COVID-19 pandemic on stroke care in Yemen.
Conclusion
During the COVID-19 pandemic, the admission rate for stroke patients declined, while the mortality rate increased. In comparison to the pre-COVID-19 period, a higher percentage of these patients arrived late, spent less time in the hospital, and had more HTN, DM, dysphasia, and altered levels of consciousness, including coma. However, similar characteristics of age, and sex were observed.
Authors’ contribution:
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; and gave final approval of the version to be published.
References
- Baker T, Schell CO, Petersen D.B et al. Essential care of critical illness must not be forgotten in the COVID-19 pandemic. Lancet 2020; 395: 1253–1254.
- Yaghi S, Ishida K, Torres J et al. SARS-CoV-2 and Stroke in a New York Healthcare System. Stroke 2020;51:2002–2011.
- Zhao J, Li H, Kung D et al. Impact of the COVID-19 Epidemic on Stroke Care and Potential Solutions. Stroke 2020; 51:1996–2001.
- Mao L, Jin H, Wang M et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020;77(6):1-9 http://doi:10.1001/jamaneurol.2020.1127.
- Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet Neurol. 2020; 19:767-83. https://doi.org/10.1016/S1474-4422(20)30221-0
- Kihira S, Schefflein J, Mahmoudi K et al. Association of coronavirus disease (COVID-19) with large vessel occlusion strokes: a case-control study. AJR 2021;216:1–6. https://doi.org/10. 2214/AJR.20.23847
- Helms J, Kremer S, Merdji H. et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med 2020. https://doi.org/10.1056/NEJMc2008597
- Lutf AQ. COVID-19 in Yemen: The present situation and the future plan to overcome the crisis. Yemen J Med. 2022;1(1):14-16.
- Kotiso M, Qirbi N, Al-Shabi K, et al. Impact of the COVID-19 pandemic on the utilisation of health services at public hospitals in Yemen: a retrospective comparative study. BMJ Open. 2022 Jan 3;12(1):e047868.
- Bersano A, Kraemer M, Touze E et al. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol 2020;27:1794-1800
- Schwarz V, Mahfoud F, Lauder L et al. Decline of emergency admissions for cardiovascular and cerebrovascular events after the outbreak of COVID-19. Clin Res Cardiol 2020: 1-7.
- Diegoli H, Magalhaes PSC, Martins SCO et al. Decrease in Hospital Admissions for Transient Ischemic Attack, Mild, and Moderate Stroke During the COVID-19 Era. Stroke 2020; 51: 2315-2321.
- Padmanabhan N, Natarajan I. Gunston R et. .Impact of COVID-19 on stroke admissions, treatments, and outcomesat a comprehensive stroke center in the United Kingdom. Neurological Sciences 2021; 42:15–20.
- Jeong HY, Lee EJ, Kang MK et al. Changes in Stroke Patients’ Health-Seeking Behavior by COVID-19 Epidemic Regions: Data from the Korean Stroke Registry. Cerebrovasc Dis, 2021; 30:1-9.
- Hsiao J, Sayles E, Antzoulatos E et al. Effect of COVID-19 on Emergent Stroke Care: A Regional Experience. Stroke 2020; 51: e2111-e2114.
- Jasne AS, Chojecka P, Maran I et al. Stroke Code Presentations, Interventions, and Outcomes Before and During the COVID-19 Pandemic. Stroke 2020; 51: 2664-2673.
- Kristoffersen ES, Jahr SH, Thommessen B, Ronning OM. Effect of COVID-19 pandemic on stroke admission rates in a Norwegian population. Acta Neurol Scand 2020;142:632-636.
- Naccarato M, Scali I, Olivo S et al. Has COVID-19 played an unexpected “stroke” on the chain of survival? J Neurol Sci 2020; 414: 116889.
- Sharma M, Lioutas V, Madsen T et al. Decline in stroke alerts and hospitalizations during the COVID-19 pandemic. Stroke Vasc Neurol 2020;5:403-405.
- Siegler J, Heslin M, Thau Let al. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis 2020; 29: 104953.
- Uchino K, Kolikonda MK, Brown D et al. Decline in Stroke Presentations During COVID-19 Surge. Stroke 2020; 51: 2544-2547.
- Samkari ET, Alkhotani AM and Siddiqui MI, Impact of COVID-19 on the rate of stroke cases at a tertiary hospital in Makkah, Saudi Arabia. Neurosciences 2021; 26 (2): 158-162, http://doi:10.17712/nsj.2021.2.20200141.
- Brunetti1 V, Broccolini A, Caliandro P, et al. Effect of the COVID-19 pandemic and the lockdown measures on the local stroke network. Neurological Sciences 2021; 42:1237–1245. https://doi.org/10.1007/s10072-021-05045-0.
- Rinkel LA, Prick JCM, Slot RER et al. Impact of the COVID-19 outbreak on acute stroke care. J Neurol 2021:268(2)403-408.
- Holmes JL, Brake S, Docherty M, Lilford R, Watson Set al. Emergency ambulance services for heart attack and stroke during UK’s COVID-19 lockdown. Lancet 2020; 395:e93–e94. https://doi.org/10.1016/S0140-6736(20)31031-X
- John S, Hussain SI, Piechowski-Jozwiak B et al. Clinical characteristics and admission patterns of stroke patients during the COVID 19 pandemic: A single center retrospective, observational study from the Abu Dhabi, United Arab Emirates. Clinical Neurology and Neurosurgery 2020;199 :106227, https://doi.org/10.1016/j.clineuro.2020.106227.
- Bojti PP, Stang R, Gunda B et al. Effects of COVID-19 pandemic on acute ischemic stroke care. A single-center retrospective analysis of medical collateral damage. Orv Hetil 2020; 161: 1395-1399.
- Frisullo G, Brunetti V, Di Iorio R et al. Effect of lockdown on the management of ischemic stroke: an Italian experience from a COVID hospital. Neurological Sciences 2020; 41:2309–2313. https://doi.org/10.1007/s10072-020-04545-9
- Teo KC, Leung WCY, Wong YK et al. Delays in Stroke Onset to Hospital Arrival Time During COVID-19. Stroke 2020; 51: 2228-2231.
- Sacco S, Ricci S, Ornello R et al. Reduced Admissions for Cerebrovascular Events During COVID-19 Outbreak in Italy. Stroke 2020;51:3746–3750. DOI: 10.1161/STROKEAHA.120.031293
- Wang J, Chaudhry SA, Tahsili-Fahadan P, Altaweel LR, Bashir S Bahiru Z, Fang Y and Qureshi AI. The impact of COVID-19 on acute ischemic stroke admissions: Analysis from a community-based tertiary care center. Journal of Stroke and Cerebrovascular Diseases 2020;29 (12): 105344. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105344
- Wallace AN, Asif KS, Sahlein DH et al,. Patient Characteristics and Outcomes Associated with Decline in Stroke Volumes During the Early COVID-19 Pandemic. Journal of Stroke and Cerebrovascular Diseases 2021; 30,(6): 105569. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105569
- Rameez F, McCarthy P, Cheng Y et al,. Impact of a Stay-at-Home Order on Stroke Admission, Subtype, and Metrics during the COVID-19 Pandemic. Cerebrovasc Dis Extra 2020;10:159–165.
- Kwan J, Bentley P, Brown M, et al. Impact of COVID-19 Pandemic on a Regional Stroke Thrombectomy Service in the United Kingdom. Cerebrovasc Dis 2020;24:1-7. DOI: 10.1159/000512603
- Policardo L, Seghieri G, Anichini R et al. Effect of diabetes on hospitalization for ischemic stroke and related in-hospital mortality: a study in Tuscany, Italy, over years 2004-2011. Diabetes Metab Res Rev. 2015;31:280-286.
- Hosseini AA, Sobhani-Rad D, Ghandehari K ey al. Frequency and clinical patterns of stroke in Iran - Systematic and critical review. BMC Neurology 2010; 10:72-81.
- Deresse B and Shaweno D. Epidemiology and in-hospital outcome of stroke in South Ethiopia. J Neurol Sci. 2015;355:138-42.
